Patricia Hidalgo M
San Ignacio-Pontificia Universidad Javeriana, Colombia
Title: Associations of time of oxygen saturation below 90% with apnea-hypopnea index (AHI) and the presence of high blood pressure (HBP) at 2640masl
Biography
Biography: Patricia Hidalgo M
Abstract
Statement of the Problem: Chronic hypoxia causes marked activation of the sympathetic nervous system and elicits systemic oxidative stress. Time of oxygen desaturation during sleep might be a risk factor for HBP and even more at higher altitudes. The purpose of this study was to describe whether the percentage of time of oxygen desaturation during a sleep study was associated with the presence of HBP or with higher AHI.
Methodology & Theoretical Orientation: We performed a descriptive study among 648 patients attending the sleep lab. Sleep studies were interpreted according to the AASM parameters and the percentage of time of oxygen saturation below 90(TS90), 80(TS80) and 70(TS70) were calculated. The presence of HBP was documented by either by patient report, recorded medication or direct measurement of blood pressure levels at the beginning and at the end of the sleep study.
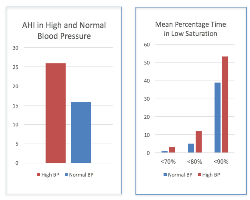
Findings: HBP was associated with higher AHI (95% confidence interval [95% CI]: 25.9(23.40, 28.55) compared to no HBP (95% confidence interval [95% CI]: 15.9(13.97, 17.98), P-value <0.0001. Being male was associated with higher AHI. TS90 were higher in patients with HBP: 58.4(95%CI =52.64, 64.29) compared to those without HBP: 40.2(95% CI= 36.52, 44.05), P-value <0.0001. The effect estimate attenuated when TS below 80 or 70 was taken into account but remained significant (P-value = 0.0012).
Conclusion & Significance: Low levels of oxygen saturation during sleep were associated with higher AHIs. Additional adjustment for lower oxygen saturation levels reduced the effect size of the association but remained significant. Further studies are needed to replicate these findings and to examine mechanisms underlying the observed association and the long-term consequences in HBP development and treatment.
References:
- Lu W, Kang J, Hu K, Tang S, et al., The role of the Nox4-derived ROS- mediated RhoA/Rho kinase pathway in rat hypertension induced by chronic intermittent hypoxia. Sleep and Breathing. Jan 2017:1-11.
- Calbet J. Chronic hypoxia increases blood pressure and noradrenaline spillover in healthy humans. Physiol.2003; 551.1, pp. 379–386.
- Almeida G, Trombetta I, Cepeda F, Hatanaka E, et al., (2017), The role of acute intermittent hypoxia in neutrophil-generated superoxide, sympathovagal balance, and vascular function in healthy subjects, Frontiers in Physiology, 2017; 8(1), Article number 4.
- Lang M, Faini A, Caravita S, Bilo G, et al., (2016), Blood pressure response to six-minute walk test in hypertensive subjects exposed to high altitude: Effects antihypertensive combination treatment International Journal of Cardiology., 219: 27-32.
- Tremblay j, Boulet L, Tymko M, Foster G., (2016), Intermittent hypoxia and arterial blood pressure control in humans: Role of the peripheral vasculature and carotid baroreflex, American Journal of Physiology-Heart and Circulatory Physiology. 311(3):699-706.



