Biography
Biography: Fabiola B Sozzi
Abstract
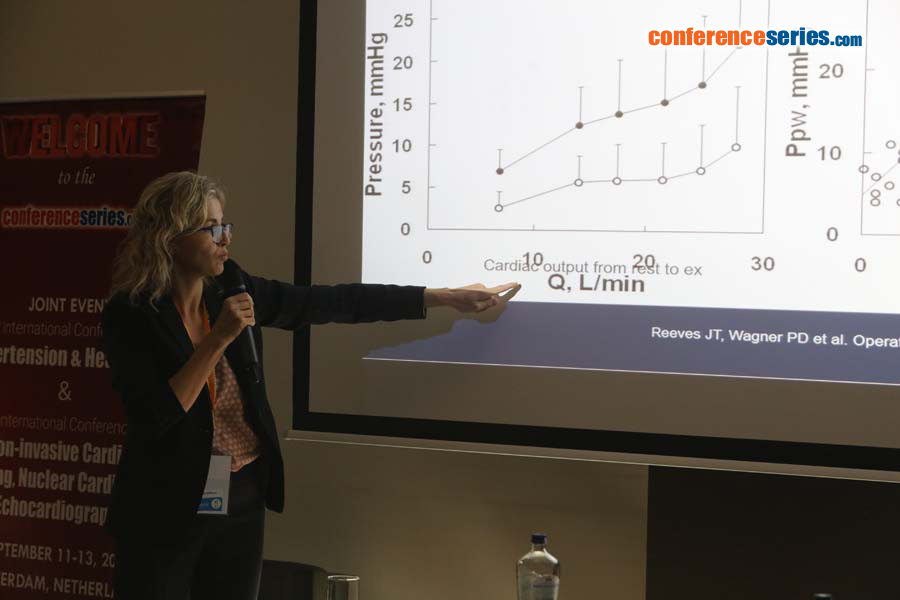
Chronic dyspnea is associated with a variety of diseases and is also a major symptom of heart failure (HF). The differential diagnosis of dyspnea is a daily routine in every cardiology practice. Approximately one-half of patients with HF have a preserved ejection fraction (HFpEF). Diagnosis of HFpEF is challenging and relies largely on demonstration of elevated cardiac filling pressures represented by the pulmonary capillary wedge pressure (1). The American College of Cardiology Foundation/American Heart Association guidelines define HFpEF as clinical signs and symptoms of HF, preserved ejection fraction, and no other obvious explanation for symptoms. This scheme works well for patients with a high likelihood of disease on the basis of clinical indicators of congestion. To address the patients without overt congestion, more recent guideline statements from the European Society of Cardiology (ESC) and American Society of Echocardiography/European Association of Cardiovascular Imaging (ASE/EACVI) [2] require objective evidence of high left ventricular filling pressures. Elevated left ventricular filling pressure is a cardinal feature of HfpEF and can be clinically demonstrated by elevations in plasma natriuretic peptide levels. The ratio of transmitral E to mitral annular e′ velocities (E/e′) at doppler echocardiography has been proposed as a non-invasive measure of left ventricular filling pressure and endorsed by professional guidelines as a surrogate parameter of invasive left ventricular filling pressure in the diagnostic work-up of HFpEF.
The diagnosis of HFpEF is straightforward when patients are acutely decompensated. To make matters more complex, many patients with HFpEF display normal left ventricular filling pressures at rest, with abnormalities that develop during stresses like exercise (3). Invasive hemodynamic exercise testing has emerged as the gold standard to diagnose or exclude HFpEF in patients with exertional dyspnea of unclear etiology, but cost, risk, and the requirement for specialized training and equipment may limit its broad application in practice and in clinical trials. Therefore, doppler echocardiography plays a central role in the non-invasive evaluation and grading of diastolic dysfunction.
References:
- Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelisa A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009; 10:165-193.
- Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur Heart J. 2011;32:670-679.
- Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200.