Day :
- Sessions
Location: Amsterdam, Netherlands
Session Introduction
Faezeh Sahbaeiroy
Iran
Title: Differences between current clinical and American Heart Association blood pressure measurement techniques
Time : 10:10-10:40
Biography:
Abstract:
Statement of the Problem: The guidelines recommended by American Heart Association for blood pressure measurement are commonly by health workers who take blood pressure. For taking blood pressure ,it is important to apply standard methods. If we do it with a few mistakes the result may be effect in patient's medication.
The purpose of this study: Is to compare the rate and accuracy of measuring blood pressure by Health Workers methods and American Heart Association Technique.
Methodology: For validation of this observation we designed a descriptive and observational study to be carried out in seven hospitals. Four hundred health workers divided into four groups (125 nurses 100 nursing students 100 medical students 75 physicians) were evaluated in a two part test. In first part (practical) the examinee had to follow all steps recommended by American Heart Association to get a passing score. In the second part (theoretical which came second to avoid influencing the practical) the examinee had to answer correctly 8 questions based on American Heart Association's guidelines to obtain a passing score.
Findings: 52.5 % of systolic and 49.3% of diastolic readings was out of range. Nursing students obtained the best practical results (52% systolic and 39% diastolic within range) and physicians obtained the lowest values (18.5% and 31.4%). These two groups showed deficiencies in the theoretical test (physicians 7.6% correct answers and Nursing students 19.5%). Medical students obtained the best results on the theoretical test (73% correct P<0.001 versus the other groups) but were deficient in the practical test (28% systolic and 42% diastolic within range).
Conclusion: In conclusion health workers used various techniques for measurement and no completely followed the standard. Such measurements may affect diagnosis and treatment of hypertension but measuring all BPs solely by the standard is not practical. We need to have a practical and efficient method for measuring BP.
Bum Ju Lee
Korea Institute of Oriental Medicine, KR
Title: Prediction of pre-hypertension and metabolic syndrome using combined obesity indices based on machine learning
Time : 11:00-11:30

Biography:
Bum Ju Lee has his expertise in evaluation in association between anthropometric indices and metabolic abnormalities. He studied the relationship between anthropometric indices related to obesity and hypertension, hypotension, type 2 diabetes, hypertriglyceridemia, and serum high- and low-density lipoproteins, and have published many articles with these contents. He is currently a senior researcher in the Korea Institute of Oriental Medicine, Daejeon, Korea. His research interests include data mining and database, bioinformatics, public health, epidemiology, and oriental medicine.
Abstract:
Statement of the Problem: Hypertension and metabolic syndrome (MetS) are a common health problem. Many previous studies reported that MetS and hypertension were strongly associated with obesity. However, no studies on the prediction of pre-hypertension and MetS using combined anthropometric indices related to obesity have been reported. The objectives of this study were to predict pre-hypertension and MetS using combined anthropometric indices based on machine learning and to evaluate the quality of various predictive models.
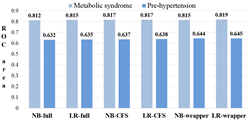
Methodology & Theoretical Orientation: A total of 3,927 subjects aged 40-70 years participated in this study. To diagnose pre-hypertension and MetS, we considered the recommendations of the National Cholesterol Education Program Adult Treatment Panel III. For anthropometric indices, eight circumferences (forehead, neck, axilla, chest, rib, waist, pelvis, and hip) were measured. We calculated the ratios between the indices. Finally, we extracted a total of 41 variables including age, weight, height, waist-to-hip ratio, waist-to-height ratio, body mass index, neck-to-rib ratio, and so on. For model building, correlation-based feature selection and wrapper-based variable selection based on logistic regression (LR) and naïve Bayes (NB) were used to identify the optimal variable subsets. Findings: There were 1,605 men with pre-hypertension (41%) and 1,136 (29%) with MetS. We tested six models in each disease (Figure 1). The LR-wrapper model showed the highest predictive power. The ROC values for the pre-hypertension and MetS were 0.645 and 0.819, respectively. In MetS, the model using combined indices showed slight improvements in the ROC compared with the waist circumference (ROC = 0.809 by NB and LR), even though waist circumference is one of the five components used to diagnose MetS and is a strong predictor of MetS.
Conclusion & Significance: Our results provide insight into a simple and inexpensive method that could be used to identify pre-hypertension and MetS in initial health screening.
References:
-
Lee BJ, Kim JY (2014) A comparison of the predictive power of anthropometric indices for hypertension and hypotension risk. PLoS One 9:e84897.
-
Asayama K, Sato A, Ohkubo T, et al. (2009) The association between masked hypertension and waist circumference as an obesity-related anthropometric index for metabolic syndrome: the Ohasama study. Hypertens Res 32:438-443.
-
Lee BJ, Ku B, Nam J, et al. (2014) Prediction of fasting plasma glucose status using anthropometric measures for diagnosing type 2 diabetes. IEEE J Biomed Health Inform 18:555-561.
-
Lee BJ, Nam J, Kim JY (2016) Predictors of metabolic abnormalities in phenotypes that combined anthropometric indices and triglycerides. BMC Complement Altern Med 16:59.
- Lee BJ, Kim JY (2016) Identification of Type 2 Diabetes Risk Factors Using Phenotypes Consisting of Anthropometry and Triglycerides based on Machine Learning. IEEE J Biomed Health Inform 20:39-46
Haben Tsehaye Ghebray
Mekane Hiwet Medical Center, Uganda
Title: Myocardial perfusion scan; A case study
Time : 11:30-12:00
Biography:
Haben Tsehaye is a medical doctor who has been practising in internal medicine and cardiology for the last 6 years. He holds his degrees from Orotta School of medicine. He is very vigilant and hardworking. He has worked in different hospitals. His passion for cardiology has enabled him to work more on this field and take care of patients with cardiac diseases. He has presented many cardiology and internal medicine cases in different occasions. His interest in publishing and research is enormous.
Abstract:
Coronary artery disease remains major health concern and leading cause of death throughout the world. Effective assessment with non-invasive test such as myocardial perfusion scan, exercise stress test and stress echocardiography with dobutamine can provide useful diagnostic and prognostic information.
Here we discuss the role of myocardial perfusion scan in 55 year old hypertensive diabetic and obese patient with exertional chest pain and shortness of breath. His baseline ECG was normal with some nonspecific ST-T changes and ECHO with EF OF 50% and no structural or regional motion wall abnormality.Patient was tried with exercise test but because of dyspnea and his obesity will hinder the echocardiography window, we stopped exercise and dobutamine echocardiography test and decided adenosine myocardial perfusion scan. The MPS scan result showed reversible ischemia in anterioseptoapical portion of the myocardium and then angiography was done and showed 90% stenosis in the mid LAD. Patient was stented with DES and started on dual antiplatelet and imporved clinically and he is doing good on his follow up and no complaint of dypnea or exertional chest pain.
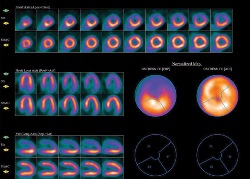
Figure1: The result of the MPS as seen above
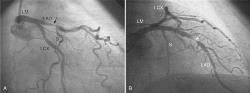
Figure 2: Angiography result of mid lad stenosis
References:
- Santos-Ocampo C D, Herman S D and Travin M I, et al. (1994) Comparison of exercise, dipyridamole, and adenosine by use of technetium 99m sestamibi tomographic imaging. Journal of Nuclear Cardiology 1:57–64.
- Henzlova M J, Cerqueira M D, Hansen C L, Taillefer R and Yao S S (2009) ASNC Announcement. Journal of Nuclear Cardiology 16:331.
- Marzilli M, Merz C N and Boden W E, et al (2012) Obstructive coronary atherosclerosis and ischemic heart disease: an elusive link. Journal of the American College of Cardiology 60:951–56.
- Hachamovitch R, Hayes S and Friedman J D, et al. (2003) Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: what is the warranty period of a normal scan, Journal of the American College of Cardiology 41:1329–40.
- Zoghbi G J, Dorfman T A and Iskandrian A E (2008) The effects of medications on myocardial perfusion. Journal of the American College of Cardiology 52:401–16.
A.J. van Ballegooijen
VU University, Amsterdam, The Netherlands
Title: The joint association of vitamin D and vitamin K with incident hypertension and cardiovascular health
Time : 12:00-12:30

Biography:
Hanne van Ballegooijen, is a nutritional-epidemiologist who is currently working at the VU University. Her main expertise is in the field of mineral metabolism disturbances and cardiovascular disease risk. After her PhD she received a personal grant (2013) to work at the Kidney Research Institute at the University of Washington, Seattle in the group of Jonathan Himmelfarb and Bryan Kestenbaum and studied nutritional determinants in chronic kidney patients. Her research interests include nutrition and lifestyle determinants in the etiology of chronic diseases. She has a particular interest in how mineral metabolism disturbances affect cardiovascular disease risk. A better understanding of these relationships may help to promote cardiovascular health.
Abstract:
Statement of the Problem: Cardiovascular disease and osteoporosis are major age-related causes of morbidity and premature death that occur among older adults. Emerging evidence suggests that calcium from bone is deposited in the arteries. This leads to calcification in valves and vessels, which is associated with a 3-4 fold higher risk of coronary heart disease. Calcium and vitamin D supplementation is frequently advised in older adults for the prevention of osteoporosis and to reduce the risk of fractures and falls. However, recent RCT's showed that individuals taking calcium and vitamin D were at higher risk of cardiovascular disease. The widespread use of vitamin D and calcium supplements, and the fortification of vitamin D in food products, underscores the need for further investigation.
Recent studies show that vitamin K reduces coronary calcification and cardiovascular disease. New evidence suggests that vitamin K combined with vitamin D can lower vascular calcification more than the effect of either alone. This presentation will give a brief overview of the current body of evidence of joint associations between vitamin D and vitamin K with hypertension and underlying mechanisms of cardiovascular disease in multiple cohort studies.
Conclusion & significance: The combination of low vitamin D and K status is associated with increased blood pressure and might play a role in development of hypertension and cardiovascular disease risk. These promising results of the joint associations of vitamin D and vitamin K in relation to cardiovascular health stimulate further follow-up studies to better understand the clinical implications of this relationship to promote cardiovascular health.
References:
-
Van Ballegooijen AJ, Rhee EP, Elmariah S, de Boer IH, Kestenbaum B., (2015), Renal Clearance of Mineral Metabolism Biomarkers. J Am Soc Nephrol, ASN 2014, 21253.
-
Van Ballegooijen, AJ, Gansevoort, RT, Lambers-Heerspink H, de Zeeuw D, Visser M, Brouwer IA, Kema IP, de Borst MH, Bakker SJ, Joosten MM.(2015), Plasma 1, 25-Dihydroxyvitamin D and the Risk of Developing Hypertension, the Prevention of Renal and Vascular End-Stage Disease Study. Hypertension; 66(3):563-70.
-
Van Ballegooijen AJ, Kestenbaum B, Sachs MC, de Boer IH, et al.,(2014), Association of 25-hydroxyvitamin D and Parathyroid Hormone with Incident Hypertension: The Multi-Ethnic Study of Atherosclerosis J Am Coll Cardiol.; S0735-1097(14)00300-3.
-
Van Ballegooijen AJ, Visser M, Cothc MF, Arai AE, et al., (2013) Serum Vitamin D and Parathyroid Hormone in Relation to Cardiac Structure and Function: the ICELAND-MI Substudy of AGES-Reykjavik. J Clin Endocrinol Metab.; 98: 2544-2552.
- Van Ballegooijen AJ, Reinders I, Visser M, Brouwer IA., (2013), Parathyroid hormone and cardiovascular disease events: A systematic review and meta-analysis of prospective studies, Am Heart J.; 165(5):655-64, 664.e1-5.
Fatemeh Esfarjani
Shahid Beheshti University of Medical Sciences, Iran
Title: Metabolic syndrome and blood pressure, predict cardio vascular risk factors in children with obesity
Time : 12:30-13:00

Biography:
Fatemeh Esfarjani is a academic member of food and nutrition policy and planing research department, in national nutrition and food technology research institute , she has years of experience in research, evaluation, teaching and administration both in hospital and education institutions. Her field of interest is in clinical nutrition, she published 23 papers in academic journals and more than 124 abstract presentations in congresses.
Abstract:
Childhood obesity increases the risk of metabolic syndrome (MetS) both in childhood and adulthood. The present study was determined the prevalence of MetS and its potential determinants in a representative sample of obese children. This cross-sectional study was conducted among 150 obese children. body mass index (BMI≥95th percentile) with seven years of age. They were randomly selected from 9 health centers in 3 districts of the north Tehran. Trained nutritionists completed a socio-demographic questionnaire by interviewing parents, and conducted the physical examination. Mets was defined based on modified ATP III criteria. The mean (SD) of weight, height, and BMI was 37.5 (6.3) kg, 127.2 (4.7) cm and 23.08 (2.9) kg/m2, respectively. The prevalence of MetS was 13.4%, without significant difference in terms of gender. The most common component of MetS was abdominal obesity (79%). While 21.3% of children did not have any component of MetS, 42% of them had at least one component. Most children with MetS had a history of breastfeeding for less than 6 months. Waist circumference, systolic and diastolic blood pressure, fasting blood glucose, and triglyceride levels were higher in Mets compared to controls (p<0.05). Logistic regression model revealed that children with birth weight of ≤2500 gr. were at higher risk of MetS than children with a higher birth weight (OR=4.3; 95%CI: 1.1-9.7). Primordial prevention of childhood obesity, screening the components of MetS among obese children and assessing the clustering of risk factors is associated with an increased risk of cardiovascular disease. Therefore, these components should be considered as a health priority at individual and public levels.
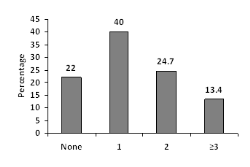
Figure 1: Frequency of obese children according to the number of metabolic syndrome components
References:
-
Kelishadi R. (2007) Childhood overweight, obesity, and the metabolic syndrome in developing countries, Epidemiologic reviews, 29 (1): 62-76.
-
Karnik S, Kanekar AS., (2011) Childhood Obesity: A Global Public Health Crisis, International Journal of Preventive Medicine, 3(1).
-
Sen Y, Kandemir N, Alikasifoglu A, Gonc N, Ozon A., ( 2008), Prevalence and risk factors of metabolic syndrome in obese children and adolescents: the role of the severity of obesity. European journal of pediatrics, 2008, 167(10): 1183-9.
-
Esfarjani F. (2012) Assessing the effect of lifestyle modification intervention in school-age obese Children. Final Report National Nutrition and Food Technology Research Institute. Tehran, Iran.
- Barzin M, Hosseinpanah F, Saber H, Sarbakhsh P, Nakhoda K, Azizi F. (2012) Gender Differences Time Trends for Metabolic Syndrome and Its Components among Tehranian Children and Adolescents. Cholesterol, 2012
Issam A Mikati
Northwestern University, USA
Title: The Use of strain imaging in detection and management of patients with early cardiomyopathy
Time : 13:00-13:30

Biography:
Issam Mikati graduated from the American University of Beirut Medical School. He did Cardiology fellowship at Baylor College of Medicine. He complaeted imaging fellowship at the same institution. He is the associate director of the Echocardiography lab at NorthwesternMemorial hospital in Chicago Illinois. He has published numerous papers in reputed journals and has served as a reviewer of premier journals.
Abstract:
Cardiomyopathy confers a poor prognosis. Early recognition and intervention is key to improve outcome. Classic methods of assessment of LV systolic dysfunction such Left Ventricular Ejection Fraction (LVEF) suffer from wide variance that limits their utility in detection of minor changes in systolic function on serial testing. In addition, the changes in LVEF appear late after significant myocardial damage has occured. This has been shown to affect prognosis of patients. Strain has been shown to be an accurate sensitive marker of LV function with leass varaiance than traditional methods of LV systolic function. It has been shown to drop early in the natural history of many systemic diease that affect the heart such as diabetic cardiomyopathy. Strain shows great promise in management of cardiomyopathies because its efficacy in early detection and potentially effects of treatment.
Toan Pham
Auckland Bioengineering Institute, New Zealand
Title: Right heart failure: consequences for the mechanical efficiency of left-and right-ventricular trabeculae from pulmonary hypertensive rats
Time : 11:45-12:15

Biography:
Toan’s research is focused on the energetics and mechanisms of the progression from hypertrophy to heart failure, using different techniques of measuring cardiac efficiency: microcalorimetry on trabeculae and respirometry on mitochondrial functions.
Abstract:
An increase in pulmonary arterial pressure increases the load on the right ventricle (RV). With time, progressive pulmonary arterial hypertension (PAH) results in RV hypertrophy, leading ultimately to right-heart failure. In contrast, PAH reduces the passive filling pressure in the left ventricle (LV). This reduces the LV workload, thereby resulting in LV atrophy. Does the structural deformation of the ventricles in right-heart failure affect their mechanoenergetic performance? To address this question, we used the PAH rat induced by a single injection of monocrotaline (MCT) (60 mg/kg) as our experimental model of right-heart failure. Six weeks after MCT injection, the hearts showed signs of right hypertrophy (indexed by increased free wall thickness) and left atrophy. Trabeculae tissue isolated from both ventricles of ‘Control’ and ‘PAH’ rats were mounted in our work-loop calorimeter, and subjected to stress-length work-loops over a wide range of afterloads while contracting at 5 Hz at 37 °C – a protocol designed to mimic the pressure-volume work of the heart. By simultaneously measuring heat production, mechanical efficiency was calculated as the ratio of work output to change of enthalpy (the sum of work and heat). The trabeculae were then required to undergo a preshortening protocol in which isometric force and heat output were measured as functions of muscle length. In right-heart failure secondary to pulmonary hypertension, RV trabeculae show a decrease in myocardial mechanical efficiency correlated with their lower stress-length work performance. The higher activation heat (ordinate of the heat-stress relationship) observed in RV trabeculae from the PAH group reflects an increased energy cost of Ca2+ cycling during contraction. In contrast, LV trabeculae from PAH group sustain normal energy efficiency over a wide range of afterloads.
Hsuan Lo
Tzu university, Taiwan
Title: Altered NMDA receptor-nitric oxide (NO) signaling in the rostral ventrolateral medulla contribute to cardiovascular response of acute ethanol-exposure
Time : 12:45-13:15

Biography:
Hsuan Lo is a PhD scholar study in the department of pharmacology and toxicology at Tzu Chi University, our lab is interested in neuropharmacology particular in alcohol effects on the central nerve system and cardiovascular function. My studies focus on the mechanism of acute ethanol intake action on the glutamate signaling within the rostral ventral lateral medulla (RVLM). I have performed the whole animal model with practiced skill in RVLM microinjection of drug and femoral artery surgery for measureing blood pressure, and also have set up the HPLC system to detect the neurotransmitter content. On the other hand, my master's thesis was studied of Amyloid-beta peptides on NMDA receptor activation in rat sympathetic preganglionic neurons using whole cell patch clamp technique. All my training have led me to know more about how the CNS works to control cardiovascular function.
Abstract:
Consumption of ethanol (EtOH) has many effects on physiological functions particular in the central nerve system and cardiovascular system. Hypotension is one of the main features of acute excessive intake of ethanol (alcohol intoxication). In addition, chronic ethanol consumption has been associated with cardiovascular diseases, including hypertension and stroke. The precise mechanisms underlying ethanol regulation of cardiovascular function remains unclear. It is well known central N-Methyl-D-Aspartate (NMDA) receptors are implicated in the modulation of glutamatergic transmission and important in regulating neuronal activity. Recent evidence also suggests that nitric oxide is a key neuromodulator within the central nervous system and its production is associated with NMDA receptor activation. The rostral ventrolateral medulla (RVLM) is known as a vasomotor center, which provides the basal sympathetic outflow and maintains blood pressure (BP). This study was carried out to test the hypothesis that NMDA and NO signalings in the RVLM are involved in the regulation of ethanol-induced changes in BP. The BP response was measured in urethane anesthetized SD rats weighing 280-350 g. EtOH (3.2 g/kg) was applied by intraperitoneal injection (IP). The samples of glutamate and NO were collected by microdialysis every 15 mins in the RVLM and then analyzed with HPLC-ECD and NOx analyzer, respectively. The results showed that IP ethanol elicited a significant increase in the level of glutamate and NO in RVLM and a reduction in BP. Microinjection of ketamine (an NMDA receptor antagonist) or L-NNA (an NOS inhibitor) into the RVLM, which was applied 5 min after administration of EtOH, attenuated EtOH-induced depressor effects. In addition, microinjection of ketamine suppressed the level of NO production. The results suggest that increases in NMDA receptors activation and enhancement of NO synthase activity in the RVLM may play a major role in ethanol-evoked hypotension.
- Sessions
Location: Amsterdam, Netherlands
Session Introduction
Fabiola B Sozzi
University of Milan, Italy
Title: When and how to perform diastolic stress echocardiography?
Time : 11:10-11:40

Biography:
Fabiola Sozzi works as a staff cardiologist at the University Hospital Policlinico of Milan, Italy, with high-specialization nomination. She has high skills in multimodality imaging of heart disease using echocardiography integrated with cardiac magnetic resonance imaging, cardiac computed tomography and nuclear. She also works in the acute clinical setting treating acute cardiac syndromes. She gained a high expertise in echocardiography at the Thoraxcentre of Rotterdam (NL), where she defended the PhD thesis on stress cardiac imaging under the supervision of Professor J. Roelandt. She is Visiting Professor at the University of Milan where she leads several research projects and teaches at the Faculty of Medicine and School of Specialization of Cardiology. She is author of 70 papers published in indexed peer-reviewed international journals and reviewer of several medical international journals.
Abstract:
While echocardiographic grading of left ventricular diastolic dysfunction is used every day, the interactions between diastolic dysfunction grade at echocardiography and the hemodynamic abnormalities are still not completely clarified (1). Collectively, there is growing evidence that the diastolic stress test can provide important diagnostic findings that can be helpful in the management of patients presenting with dyspnea of an unclear etiology. Many patients present with exertional dyspnea and exercise intolerance, but have normal left ventricular filling pressures at rest. In these patients, it is important to evaluate filling pressure with exercise. Exercise can be performed using a supine bicycle or treadmill protocol. Alternatively dobutamine can be used, though its vasodilator as well as inotrope effect determine a very different hemodynamic response compared to that of exercise. We need to record mitral inflow by pulsed doppler echocardiography at the level of the mitral tips, mitral annular velocities by spectral Doppler echocardiography, and tricuspid regurgitation jet by continuous-wave Doppler at baseline and after the termination of exercise. Diastolic function parameters can be obtained after the assessment of regional wall motion abnormalities, especially when an exercise echocardiogram is performed for the evaluation of dyspnea. In patients with diastolic heart failure, left atrial pressure is increased, leading to an increase in mitral E velocity, whereas annular e’ velocity remains reduced given the limited preload effect on e’. Moreover, an increase in the pulmonary artery systolic pressure can be detected by the increase in peak velocity of the tricuspid regurgitation jet (2). On the other hand, in the absence of cardiac disease, e’ increases to a similar extent to the increase in mitral E velocity, and the normal E/e’ ratio essentially is unchanged with exercise (3). The concept of the diastolic stress test were introduced more than 10 years ago. Subsequently, exercise E/e’ ratio was validated against invasive measurements. Importantly, exercise septal E/e’ ratio was an important determinant of exercise capacity, and its decline with age was noted in a large series of patients referred for exercise echocardiography. Furthermore, a recent study showed the incremental prognostic value of exercise E/e’ ratio over clinical variables and exercise wall motion score index.
In conclusion, diastolic stress test has an interesting role in patients with heart failure and preserved ejection fraction that present symptoms during activity, normal ejection fraction and inconclusive diastolic function at rest.
References:
- Oh JK, Park SJ, Nagueh SF. Established and Novel Clinical Applications of Diastolic Function Assessment by Echocardiography. Circ Cardiovasc Imaging 2011;4:444-445
- Kane GC, Oh JK. Diastolic Stress Test for the Evaluation of Exertional Dyspnea. Curr Cardiol Rep 2012;14:359-365
- Ratanasit N, Karaketklang K, Chirakarnjanakorn S, Krittayaphong R, Jakrapanichakul D. Left atrial volume as an independent predictor of exercise capacity in patients with isolated diastolic dysfunction presented with exertional dyspnea. Cardiovascular Ultrasound 2014,12:19-26
Vladimir A.Mikhaylov
Eternity Medicine Institute, Dubai
Title: Newly discovered way of the function of cardio-vascular system and the latest theory of the development of hypertension and other cardiovascular diseases
Time : 11:40-12:10

Biography:
1982 - After receiving his medical degree from the Ryazan medical institute named after I.P. Pavlov (M.D.) protected a degree of Ph.D. (Formation dublical anastomosis in surgery of intestinum and pancreas. 1994 - received a degree Sci.D. in National center of laser medicine in Moscow (Use of low- level of laser radiation in treatment of oncology diseases. 1997 - Ðead of Moscow Scientific-Practical Center of laser Medicine. 1999 - selected in Board of directors (EMLA), direction – oncology and angiology in Vienna, Austria. 2001- President of the VIIIth Congress of European Medical Laser Association (EMLA), Moscow, Russia. The member of international editorial board of the “Laser Therapy”. 2009 - Has been recognized as an International Medical Laser Specialist at class: Hon-IMeLas, Number: H-0017, Congress ISLSM, WFSLMS, Tokyo, November 27, 2009. 2013 - Physician Contract with Eternity Medicine Institute, Dubai, Social activity. 2015 - Award winner - Ming Chien Kao Awards 2015 (For publishing article- . Use of intravenous laser blood irradiation (ilbi) at 630-640 nm to prevent vascular diseases and to increase life expectancy. Laser Therapy, vol 24(2015), No.1, p.15-26).
Abstract:
Statement of the Problem: It is known that the power of the heart alone is about 3.3 W, and the length of the vessels is about 100,000 km. It made us doubt that with this power the heart can deliver blood to the capillary bed. Effects on the vascular wall of various modes of laser radiation (wavelength of 630-640 nm.) showed that if continuous radiation did not affect the parameters of blood pressure, frequency regimes had an impact. This leads us to the idea that the root cause of the development of different cardiovascular diseases is the system disturbance of the activity of the vascular pump leads to the increase of intra vascular pressure and the emergence of the hypertensive illness and the coronary heart disease.
Theoretical Orientation: To confirm this idea that the main role in the delivery of blood to tissues primarily played by the vessels and not the heart, we conducted the following studies: 1. Built a new mathematical model. 2. Changed features of the anatomical structure of different types of arteries. 3. Explained how the synchronization of the heart and blood vessels transporting blood to the tissues.
Conclusion & Significance: The main role in transportation of blood to the capillary bed play an artery, the power of the heart is only 0,49 -0,027% of the power needed to transport blood to the capillary bed. The vascular pump is regulated by the frequency of contractions of the heart muscle and is tightly synchronized with the work of the heart. The rapid spread of the pulse wave creating a suction effect. Following the reduction of the vessel wall, the blood just drawn from the aorta and large arteries to the smaller vessels down to the capillary bed. Systematic irregularities in the vascular pump are the starting point in the development of hypertension. These illnesses may be both local and systemic, depending on the size and location of pathological changes in the vascular wall.
Recommendations: It is necessary to conduct further studies to confirm the mechanisms of development of hypertension.
References:
- McDonald, D.A.: Blood flow in arteries. Second ed. London: Arnold 1974.
- GUYTON, A.C., YOUNG, D.B. (Eds): Cardiovascular Physiology III, Vol. 18, Baltimore: University Park Press, 1979.
- Mikhaylov V.A., (2007) Intravenous laser blood irradiation, Greece, 2007, 102 p.
- Mikhaylov V.A., (2015), Use of intravenous laser blood irradiation (ilbi) at 630-640 nm to prevent vascular diseases and to increase life expectancy. Laser Therapy, vol 24, No.1, p.15-26
- Mikhaylov V.A., (2016) Ming Chien Kao Awards 2015, Laser Therapy, mar 2016, vol. 25, No.1, p.9-10.
Valéria Paula S. Fazan
University of São Paulo ,Brazil
Title: Evidence of a hypertensive peripheral neuropathy in an experimental model of hypertension in rats
Time : 14:10-14:40

Biography:
Valéria Paula Sassoli Fazan graduated in the School of Medicine of Ribeirão Preto, University of São Paulo, in 1991 and attended the Neurosurgery Residency Program at the same University. Obtained the M.S. Degree in Morphology in 1995 and Ph.D. Degree in Neurology in 1999, both in the the School of Medicine of Ribeirão Preto. Currently is an Associate Professor in the Department of Surgery and Anatomy and Manager of the Microsopy and Morphometry Laboratory at the Experimental Surgery Center in the School of Medicine of Ribeirão Preto, University of São Paulo. Proficient with a wide-range of light and electron microscopy techniques including specimen preparation and handling, vacuum evaporation and autoradiography, light microscopy including brightfield, darkfield, phase, fluorescence and transmission electron microscopy including brightfield and darkfield. Expert in neuroscience, particularly in the fields of peripheral nerves and experimental models of neuropathies, digital image processing and analysis, stereology and morphometry.
Abstract:
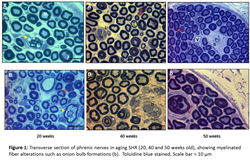
Statement of the Problem: Spontaneously hypertensive rats (SHR), first inbred from Wistar Kyoto rats (WKY), are considered a good experimental model of human essential hypertension. Hypertension is a main risk factor for stroke and vascular dementia and may cause important changes to the cerebrovascular tree, turning the brain more susceptible to infarcts, microaneurysms and ischemia. In spite of the well documented influence of hypertension on the brain, data on the sensitivity of peripheral nerves in hypertension is scarce. The purpose of this study was to investigate the alterations on the morphology and morphometric data on sural, phrenic and vagus nerves of adult SHR, with well-established hypertension.
Methodology & Theoretical Orientation: Male and female SHR and normotensive WKY rats aged 20 weeks (N = 6 in each group) were investigated. After arterial pressure and heart rate recordings in anesthetized animals, right and left sural nerves were removed and prepared for epoxy resin embedding and light microscopy. Morphometric analysis was performed with the aid of computer software, and took into consideration the fascicle area and diameter, as well as myelinated fiber number, density, area and diameter.
Findings: Significant differences were observed for the myelinated fiber number and density, comparing different genders of WKY and SHR in all nerves. Also, significant differences for the morphological (thickening of the endoneural blood vessel walls and lumen reduction) and morphometric (myelinated fibers diameter and G ratio) parameters of myelinated fibers were identified.
Conclusion & Significance: Morphological exam of the myelinated fibers suggested the presence of a neuropathy due to hypertension in both SHR genders. These results indicate that hypertension altered important morphometric parameters related to nerve conduction in hypertensive animals. Moreover the comparison between males and females of WKY and SHR showed that the morphological and morphometric alterations due to hypertension are not gender related.
References:
- Da Silva GA, Mendes VA, Genari AB, Castania JA, Salgado HC, Fazan VPS (2016), Recurrent laryngeal nerve alterations in developing spontaneously hypertensive rats. Laryngoscope 126(1):E40-7
- Sanada LS, Tavares MR, Sato KL, Ferreira R da S, Neubern MC, Castania JA, Salgado HC, Fazan VPS (2015) Association of chronic diabetes and hypertension in sural nerve morphometry: an experimental study. Diabetol Metab Syndr 7:9.
- Oliveira FS, Nessler RA, Castania JA, Salgado HC, Fazan VPS (2013), Ultra structural and morphometric alterations in the aortic depressor nerve of rats due to long-term experimental diabetes: effects of insulin treatment. Brain Res 1491:197-203.
- Sanada LS, da Rocha Kalil AL, Tavares MR, Neubern MC, Salgado HC, Fazan VPS (2012), Sural nerve involvement in experimental hypertension: morphology and morphometry in male and female normotensive Wistar-Kyoto (WKY) and spontaneously hypertensive rats (SHR). BMC Neurosci 13:24
- Rodrigues AR, Ferreira RS, Salgado HC, Fazan VPS (2011) Morphometric analysis of the phrenic nerve in male and female Wistar-Kyoto (WKY) and spontaneously hypertensive rats (SHR). Braz J Med Biol Res 44(6): 583-591.
Nilda Espinola-Zavaleta
National Institute of Cardiology Ignacio Chavez, Mexico
Title: The Polymorphism LDB3 rs (45618633), TAZ rs (104894941), LMNA (rs28928903), DTNA (rs7243528) and TNNT2 G/T (rs 2365652) and its associate with non compacted cardiomyopathy in Mexican Mestizo family
Time : 14:40-15:10

Biography:
Nilda Espinola-Zavaleta is a Cardiologists and echocardiographist of the National Institute of Cardiology “Ignacio Chavez” in Mexico City. She is a national researcher and her work is focused in pulmonary hypertension, right venricular function, congenital heart disease, ischemic heart disease, valvular heart disease, cardiomyopathies and new techniques of echocardiography.
Abstract:
Background: Noncompacted cardiomyopathy (NCC) has been attributed to the mutation in multiple genes leading to interruption in the endomyocardial compaction process. In the affected families, associations with mutations without T gene of cardiac troponin (TNNT2) and of the genes LDB3, MYH7 and ACTC, dystrobrevin (DTNA) and tafazzin (TAZ) in some with recessive inheritance and others of dominant type were found.
Objective: The objective of this work was to identify gene variants that participated in the development of NCC in a Mexican mestizo family.
Material and methods: A total of 36 (85.7%) individuals from a family of 42 members were studied. All patients underwent clinical history, transthoracic echocardiography (according to the criteria of Jenni et al) and the polymorphisms: LDB3, TAZ, LMNA, DTNA and TNNT2 G/T were obtained from whole blood through a commercial kit (WizardGenomic DNA Isolation Kit: Promega, Wisconsin).
Results: The NCC was present in 36.1% of the patients. Seven are first-generation relatives, of whom 6 presented NCC. Thirty-three second-generation relatives of whom 6 patients were positive for the disease and 2 third-generation individuals without NCC. When evaluating those with NCC vs those without NCC, differences in diastolic diameter, systolic diameter, left atrium size, left ventricuar ejection fraction, and pulmonary artery systolic pressure were found. The 100% of patients with NCC presented the A and C alleles in the polymorphisms (rs 45618633) of the LDB3 gene and (rs 104894941) of the TAZ gene. While, for the GG and TT genotype in LMNA polymorphisms (rs 28928903) and DTNA (rs 7243528) no patients with NCC were found. At follow-up, 4/13 patients with ventricular noncompaction died.
Conclusions: 36.1% of patients in the Mexican mestizo family studied developed NCC and 100% presented the A and C alleles in the polymorphisms (rs 45618633) of the LDB3 gene and (rs 104894941) of the TAZ gene. At follow-up, 30.7% of patients with NCC died.
References:
1. Maron BJ, Towbin JA, Thiene G, Antzelevitch et al. Contemporary definitions and classication of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2006;113:1807-16.
2. Monserrat L, Hermida-Prieto M, Fernandez X, Rodriguez I, Dumont C, Cazon L et al. Mutation in the alpha-cardiac actin gene associated with apical hypertrophic cardiomyopathy left ventricular non-compaction, and septal defects. Eur Heart J 2007;28:1953–1961.
Patricia Hidalgo M
San Ignacio-Pontificia Universidad Javeriana, Colombia
Title: Associations of time of oxygen saturation below 90% with apnea-hypopnea index (AHI) and the presence of high blood pressure (HBP) at 2640masl
Time : 16:15-16:45
Biography:
Alvaro Ruiz and Patricia Hidalgo have their expertise in internal medicine, clinical epidemiology and sleep disorders at high altitudes. They have built their way of focusing after years of experience in medical practice, research and teaching both in hospital and education institutions. They are research seed leaders and have population based published papers and also health guidelines.
Abstract:
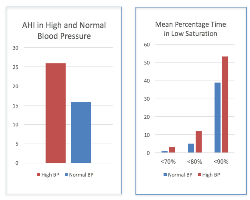
Statement of the Problem: Chronic hypoxia causes marked activation of the sympathetic nervous system and elicits systemic oxidative stress. Time of oxygen desaturation during sleep might be a risk factor for HBP and even more at higher altitudes. The purpose of this study was to describe whether the percentage of time of oxygen desaturation during a sleep study was associated with the presence of HBP or with higher AHI.
Methodology & Theoretical Orientation: We performed a descriptive study among 648 patients attending the sleep lab. Sleep studies were interpreted according to the AASM parameters and the percentage of time of oxygen saturation below 90(TS90), 80(TS80) and 70(TS70) were calculated. The presence of HBP was documented by either by patient report, recorded medication or direct measurement of blood pressure levels at the beginning and at the end of the sleep study.
Findings: HBP was associated with higher AHI (95% confidence interval [95% CI]: 25.9(23.40, 28.55) compared to no HBP (95% confidence interval [95% CI]: 15.9(13.97, 17.98), P-value <0.0001. Being male was associated with higher AHI. TS90 were higher in patients with HBP: 58.4(95%CI =52.64, 64.29) compared to those without HBP: 40.2(95% CI= 36.52, 44.05), P-value <0.0001. The effect estimate attenuated when TS below 80 or 70 was taken into account but remained significant (P-value = 0.0012).
Conclusion & Significance: Low levels of oxygen saturation during sleep were associated with higher AHIs. Additional adjustment for lower oxygen saturation levels reduced the effect size of the association but remained significant. Further studies are needed to replicate these findings and to examine mechanisms underlying the observed association and the long-term consequences in HBP development and treatment.
References:
- Lu W, Kang J, Hu K, Tang S, et al., The role of the Nox4-derived ROS- mediated RhoA/Rho kinase pathway in rat hypertension induced by chronic intermittent hypoxia. Sleep and Breathing. Jan 2017:1-11.
- Calbet J. Chronic hypoxia increases blood pressure and noradrenaline spillover in healthy humans. Physiol.2003; 551.1, pp. 379–386.
- Almeida G, Trombetta I, Cepeda F, Hatanaka E, et al., (2017), The role of acute intermittent hypoxia in neutrophil-generated superoxide, sympathovagal balance, and vascular function in healthy subjects, Frontiers in Physiology, 2017; 8(1), Article number 4.
- Lang M, Faini A, Caravita S, Bilo G, et al., (2016), Blood pressure response to six-minute walk test in hypertensive subjects exposed to high altitude: Effects antihypertensive combination treatment International Journal of Cardiology., 219: 27-32.
- Tremblay j, Boulet L, Tymko M, Foster G., (2016), Intermittent hypoxia and arterial blood pressure control in humans: Role of the peripheral vasculature and carotid baroreflex, American Journal of Physiology-Heart and Circulatory Physiology. 311(3):699-706.
Amar Mohanrao Taksande
Jawaharlal Nehru Medical College, India
Title: Evaluation of neonatal echocardiography in the neonatal intensive care unit
Time : 16:45-17:15

Biography:
Amar Taksande is presently working as Professor in Dept. of Pediatrics, at Jawaharlal Nehru Medical College (JNMC), DMIMS, Sawangi. He completed his residency at Mahatma Gandhi Institute of Medical Sciences (MGIMS) Medical College, Sevagram where he also worked as Associate Professor in the Pediatric Department. He got Fellowship in Pediatric Cardiology at Innova children heart hospital, Hyderabad. He received an award of Visiting Fellowship by Royal College of Pediatric and Child Health (RCPCH), United Kingdom. He has published over 135 papers in national and inter-national journals and is author of several paediatrics titles. He is life member of Indian Academy of Pediatrics, Pediatric Cardiology Society of India and several other medical organizations. He is also a peer reviewer of international Journals like congenital heart disease, Journal of Pediatrics, Journal of Pediatric Infectious disease etc.
Abstract:
Introduction: Congenital Heart Disease (CHD) is the most common congenital problem that accounts for up to 25% of all congenital malformations that present in the neonatal period and is leading cause of neonatal and infant mortality. Echocardiography is an investigation that is currently being used in many neonatal intensive care units (NICU) to evaluate disease progress, assist in procedural interventions, assess the functional or structural defects of the critically ill neonates at the bedside.
Objective: To evaluate the role of neonatal echocardiographic examination in the clinical management of the sick neonate in NICU.
Material and Methods: Study was conducted in the NICU of Paediatric department of a Rural Medical College in Central India over a period of 2 years. Information about all echocardiograms performed in the neonatal unit was collected prospectively. Indications for performing echocardiography, echocardiographic findings, and any resulting changes in clinical management were determined.
Results: A total of 231 echocardiograms were performed in 182 neonates. Echocardiography identified 74 neonates with a structural cardiac abnormality. Patent oval foramen and hemodynamically nonsignificant patent arterial duct (20%) and physiologic pulmonary artery stenosis (2%) were categorized as normal structural group. In addition, 11 neonates were found to have an important functional abnormality. Murmurs (55%) followed by extracardiac anomalies and dysmorphic features (32%) were the most common clinical indications for requesting an echocardiogram. Echocardiography prompted a specific change in clinical management in 72% neonates. Murmur in our critically ill neonates has been associated with a higher incidence of cardiac disease.
Conclusion: Bedside echocardiography had provided crucial information and accurate decision makings that was not apparent on clinical assessment. Hence, echocardiography is an important tool for diagnosis of cardiac abnormalities that can influence the management and outcome of the sick newborn in the intensive care unit.
Keywords: Cardiovascular malformation, congenital heart defects, Echocardiography, Neonates
- Sessions
Location: Amsterdam, Netherlands
Session Introduction
Soha M. Abd El Dayem
National Research Centre, Egypt
Title: Relationship of nitric oxide genotype to diabetic nephropathy and atherosclerosis of type 1 diabetic patients
Time : 11:05-11:35

Biography:
Soha Abd El Dayem is working in the Medical Service Unit in National Research Center as a Consultant of Diabetes and Endocrinology. She is also working in Health Insurance as a Consultant of Diabetes and Endocrinology. She is a consultant of Pediatrics in Suzan Moubarak Hospital. She is the member of Society of Egyptian Society of Cardiology.
Abstract:
Objective: Assessment of nitric oxide genotype in diabetic patients and to evaluate its relationship to diabetic nephropathy and atherosclerosis of type 1 diabetic patients.
Patients and methods: The study included 65 type 1 diabetic patients and 30 age and sex matched healthy volunteers. The mean age of patients was 17.99 ± 2.59, mean duration of diabetes was 10.91 ± 3.54, mean onset of disease was 7.00 ± 3.28. Blood samples were taken for assessment of glycosylated haemoglobin (HbA1), lipid profile, oxidized low-density lipoprotein (OxLDL) and serum level of nitric oxide by enzyme linked immunosorbent assay (ELISA) technique. Also, nitric oxide genotype was done. Urine samples were taken for assessment of albumin/creatinine ratio. Carotid intima-media thickness (cIMT) and renal dopplar via ultrasound were also done.
Results: Nitric oxide was significantly lower, while lipid profile, OxLDL and albumin/creatinine ratio, cIMT and resistivity index were significantly higher in diabetic patients. No significant difference of nitric oxide genotype was found in diabetics and control. Nitric oxide was significantly lower, while OxLDL, albumin/ creatinine ratio and lipid profile were significantly higher in nitric oxide homozygous genotype.
Conclusion: Diabetic patients had a low level of nitric oxide and early atherosclerosis. Nitric oxide homozygous genotype is associated with diabetic nephropathy and atherosclerosis.
Ahmed A. Battah
Cairo University, Egypt
Title: Apelin, nitric oxide and vascular affection in adolescent type 1 diabetic patients
Time : 11:35-12:05

Biography:
Ahmed Abdelrahman Battah is a Professor of Critical Care Cardiology Cairo University. He is working as Interventional Cardiology & Echocardiography Consultant at Cairo University hospitals & Al Salam International Hospital. He is also the member of the European society of Cardiology, Member of the European Critical Care, Member of the Egyptian Society of Critical Care Medicine, Member of the Egyptian Society of Cardiology
Abstract:
Objective: We are aiming to evaluate apelin and nitric oxide (NO) in type 1 diabetic patients and its relation to vascular affection.
Patients and methods: The study included 62 type 1 diabetic patients and 30 healthy volunteers of the same age and sex. Blood samples were taken for assessment of apelin, NO, glycosylated hemoglobin, and lipid profile. Urine samples were taken for assessment of albumin/creatinine ratio flow mediated dilatation (FMD) via ultrasound was done.
Results: The mean age of diabetic patients were 16.3 ± 1.5 yrs (14.0 – 19.0 yrs), and mean duration of diabetes were 9.4 ± 2.9 yrs (5.0 – 16.5 yrs). FMD and FMD/ nitrate mediated dilatation (NMD) ratio were significantly lower in diabetics. Nitric oxide was significantly lower, while apelin and albumin/ creatinine ratio were significantly higher than controls. No significant correlation was found between apelin, NO, FMD, albumin / creatinie ratio or BMI.
Conclusion: Diabetic patients had endothelial dysfunction and elevation of apelin, but they does not related to each other. BMI had no relation to apelin which indicate that obesity had no role to apelin. Further large study is recommended to detect the relationship of apelin with vascular affection by assesseing large numer of diabetics with and without complication.
Alan Fleming
Optos, Dunfermline, UK
Title: A proposed study in detection of hypertension by ultra-widefield ophthalmic imaging
Time : 12:05-12:35

Biography:
The authors have many years experience in developing algorithms for retinal image analysis in industry and academia. Alan Fleming has many publications in this field from University of Aberdeen. Gavin Robertson completed his PhD at University of Edinburgh in retinal vascular analysis. Jano van Hemert has led multidisciplinary research groups in academia and industry and is an ardent exponent in the commercialisation of research output.
Abstract:
Statement of the Problem: Ophthalmic imaging may provide a method for hypertension detection. Changes to the caliber of the retinal vasculature near the optic disc are early biomarkers of hypertension. We hypothesize that changes in vessel caliber in ultra-widefield scanning laser ophthalmoscope (UWF-SLO) images can be used to classify hypertensive status.
A pilot study with 500 subjects has shown that software (optomapHT, Optos, UK) for semi-automated detection of venular and arteriolar caliber in UWF-SLO images can predict hypertensive status, defined by clinical blood pressure (BP) >= 140mmHG, area under receiver operator characteristics curve (AUROC) of 0.720.
Proposed study aim: To determine the ability of optomapHT to predict hypertensive status as established through either ambulatory BP measurement or clinical BP measurement.
Study design: Ambulatory BP measurements provide a better prediction of retinal arteriole caliber than clinical BP. However, the procedure for ambulatory BP measurement may cause discomfort for the patient making population based studies difficult. Therefore, the proposed study participants will be patients whose routine care includes either ambulatory BP or clinical BP measurement. Informed consent will include agreement to undertake, in addition, UWF-SLO retinal imaging. Outcome measures will be AUROC for the prediction by optomapHT of hypertension according to clinical BP or ambulatory BP. To show that optomapHT is at least equivalent to clinical BP for diagnosis of hypertensive status 600 participants are required,.
Conclusion: In addition to eye care, UWF-SLO imaging technology presents an opportunity for early detection of hypertensive patients. Collaborators in this study would benefit from partnership with a highly successful ophthalmic imaging company.
Ahmed A. Battah
Cairo University, Egypt
Title: Glycemic control and carotid intimal medial thickness in adolescents type 1 diabetic patients : a three years follow up
Time : 12:35-13:05

Biography:
Ahmed Abdelrahman Battah is a Professor of Critical Care Cardiology Cairo University. He is working as Interventional Cardiology & Echocardiography Consultant at Cairo University hospitals & Al Salam International Hospital. He is also the member of the European society of Cardiology, Member of the European Critical Care, Member of the Egyptian Society of Critical Care Medicine, Member of the Egyptian Society of Cardiology
Abstract:
Objective: To assess carotid intimal medial thickness (cIMT) in type 1 diabetic patients who were followed up for 3 years to shed further light on relationship of glycemic control and cIMT.
Patients and methods: It is a prospective cohort observational study, included 40 type 1 diabetic patients and 30 age and sex matched healthy volunteer. Blood sample was taken for analysis of glycosylated hemoglobin (HbA1), lipid profile and urine sample was taken for analysis of albumin/ creatinine ratio. cIMT via ultrasound was also done. Three years later, patients were subjected to the original laboratory investigation and cIMT. t- test and MacNemar test was used for analysis of data.
Results: cIMT were significantly higher in diabetics in the original study. Three years later, patients had significant increase in waist/ hip ratio, HbA1, albumin/ creatinine ratio and cIMT. cIMT regressed in 3 patients, remained stationary in 18 patients (2 patients remain normal and 16 had increased cIMT) and the remaining 19 patients had progressed cIMT. Patients with progressed cIMT had significantly higher waist/ hip ratio, HbA1and albumin/ creatinine ratio than patients with stationary cIMT.
Conclusion: Adolescent type 1 diabetic patients had increased cIMT. Progression in cIMT is associated with obesity, poor glycemic control and nephropathy. We recommend good glycemic control and frequent follow up of diabetic patients for early detection of diabetic complication.
Soha M. Abd El Dayem
National Research Centre, Egypt
Title: Relationship of plasma level of nesfatin, chemerin and vaspin to early atherosclerotic changes and its genetic study in adolescent type 1 diabetic patients
Time : 13:05-13:35

Biography:
Abstract:
Objective: To evaluate the relationship of plasma level of nesfatin, chemerin and vaspin to early atherosclerotic changes. Also to evaluate chemerin and vaspin genotype and to detect its relation to glycemic control and atherosclerosis in adolescent type 1 diabetic patients.
Patients and methods: The study included 70 type 1 diabetic patients and 30 age and sex matched healthy volunteers. The mean age of patients was 17.99 ± 2.59, mean duration of diabetes was 10.91 ± 3.54, mean onset of disease was 7.00 ± 3.28. Blood samples were taken for assessment of chemerin, nesfatin, vaspin, and oxidized low-density lipoprotein (OxLDL) by enzyme linked immunosorbent assay (ELISA) technique. Also, blood samples were taken for analysis of glycosylated hemoglobin (HbA1); lipid profiles and urine samples were taken for assessment of albumin/creatinine ratio. Carotid (cIMT) and aortic (AIMT) intima-media thickness were also done.
Results: Nesfatin, chemerin, vaspin, OxLDL, albumin/creatinine ratio, cIMT and AIMT were significantly higher in diabetic patients. HbA1 and cIMT were significantly higher in homozygous (TT) genotype of chemerin than GG genotype (9.50 ± 1.99 vs 8.34 ± 1.62 and 0.54 ± 0.06 vs 0.50 ± 0.04 respectivelly). Chemerin and vaspin had a significant positive correlation (r = 0.2, P = 0.05), nesfatin and LDL (r = 0.3, P = 0.05) and Vaspin and body mass index (r = 0.3, P = 0.01). Conclusion: Diabetic patients had increased level of adipocytokines and are liable for early atherosclerosis. Homozygous genotype (TT) of chemerin in diabetic patients is associated with poor glycemic control and early atherosclerosis.
- Young Research Forum
Location: Amsterdam, Netherlands
Session Introduction
Ayush Shrivastava
Jawaharlal Nehru Medical College, India
Title: Study of tissue doppler imaging (TDI) for myocardial velocity in Sickle-Cell disease children
Time : 17:15-17:30

Biography:
Ayush Shrivastava belong to Bhopal, Madhya Pradesh, India had done undergraduate from People’s College of Medical Science and research center, Bhanpur, Bhopal and is doing residency in Paediatrics from Jawaharlal Nehru Medical College, Sawangi, Wardha, Maharashtra.
Abstract:
Background: Sickle-cell disease (SCD) is an inherited haemoglobin childhood disorder, frequently complicated by pulmonary hypertension and cardiac involvement. Tissue Doppler imaging is the simple indices for the assessment of the cardiac function.
Aim: To evaluate cardiac function by means of echocardiography in SCD children.
Study Design: Case control study
Methods: 30 children with SCD were compared with 30 age-matched healthy controls. Myocardial wall motion velocities at the lateral mitral annulus and the junction between the medial mitral annulus and the interventricular septum were assessed during systole (Sa), early diastole (Ea), and late diastole (Aa) through a four-chamber view using pulsed doppler echocardiography. The ejection fraction and shortening fraction were also estimated.
Results: The early diastolic trans-tricuspid peak flow velocity was greater in the SCA patients than in the controls. Assessment of the lateral mitral and tricuspid annulus peak velocities by pulsed TDI showed that the patients had significantly greater systolic, and early and late diastolic velocities than the controls. The left ventricular diameter, interventricular septum diameter, and posterior wall diameter were statistically significantly greater in the SCD children compared with the control group, whereas there was no difference in ejection fraction. There was a significant difference in Sa(m) wave velocity between the two groups (p < 0.042).
Conclusion: SCD in children results in a dilated heart with increase in left ventricular dimensions. TDI appears to be more sensitive in the early detection of myocardial dysfunction in SCD children.
Shreyas Rajendra Borkar
Jawaharlal Nehru Medical College, India
Title: Study of myocardial function assessment by tissue doppler imaging in neonates
Time : 17:30-17:45
Biography:
Shreyas Borkar completed my MBBS from Goverment Medical College, Nagpur under MUHS University, Nashik. He is currently pursuing his post-graduation in Department of Pediatrics in JNMC, Sawangi Meghe, Wardha, Maharashtra, India.
Abstract:
Background: In both term and premature neonates, changes in the systolic and diastolic function of the left ventricle (LV) and right ventricle (RV) reflect the degree of neonatal myocardial immaturity and the co-existence of foetal circulation as well as the presence of concurrent diseases.
Aim: To measure the ventricular myocardial velocities using tissue doppler imaging (TDI) in the neonates.
Study Design: Prospective observational study
Material and Methods: Left and right ventricular peak systolic (S'), early diastolic (E') and late diastolic (A') myocardial velocities were measured using TDI alongside standard echocardiography. E/E' ratio was calculated for both ventricles. 20 neonates were prospectively recruited into two groups: Term (n=20) and preterm (<37 weeks, n=20)
Results: The diastolic myocardial velocities recorded in the RV were higher than those in the LV. Myocardial velocities increased in term child as compared to preterm child. Left E/E' ratio was higher than right in each group.
Conclusions: In neonates, the diastolic and systolic function recorded in the RV was better than that in the LV. Also, TDI is feasible in preterm neonates and enables the acquisition of myocardial velocities.
Mrudul Kumar
Jawaharlal Nehru Medical College, India
Title: Tissue Doppler Imaging (TDI) for evaluation of cardiac functions in infants of diabetic mothers (IDM)
Time : 17:45-18:00

Biography:
Mrudul Kumar, completed his MBBS from Bhaskar Medical College and General hospital, Hyderabad, NTR University of Health Sciences. He is currently pursuing post-graduation in the Department of Paediatrics (Second Year), from Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi (Meghe), Wardha, Maharashtra
Abstract:
Introduction: Congenital anomalies occur more commonly in infants born to diabetic mothers, and cardiac defects predominate. Infant of Diabetic Mothers often develop respiratory problems which need to be differentiated from the cardiovascular problems. Transient cardiac hypertrophy occurs in infants of diabetic mothers.
Aim: To evaluate the cardiac functions by using Tissue Doppler Echocardiography in IDM.
Study Design: Case-Control Study
Material and Methods: Right and left ventricle systolic and diastolic functions of 15 term IDM and 15 healthy term newborns (control) were examined using TDI. Systolic (S'), early diastolic (E'), and late diastolic (A') TDI velocities were measured at the mitral valve (MV) annulus, basal interventricular septum (IVS), and tricuspid valve (TV) annulus. Demographic, perinatal, and echocardiographic variables were compared between IDM and control groups.
Results: IDMs groups had significantly greater birth weight, lower gestational age, older maternal age, and higher incidence of maternal obesity and hypertension than controls (p < 0.001). The septum was found to be thick in 5 (33.33%) of the IDM. Both the left and right ventricle myocardial velocities were found to be lower in the IDMs compared to the control group. Em/Am ratio was found to be less than one only in IDMs in the left ventricle in contrast to the control group.
Conclusion: Tissue Doppler Imaging demonstrated that IVS in IDM disrupt the diastolic function of both ventricles.
Toan Pham
Auckland Bioengineering Institute, New Zealand
Title: Right heart failure: Consequences for the mechanical efficiency of left-and rightventricular trabeculae from pulmonary hypertensive rats
Time : 18:00-18:15

Biography:
Toan Pham is doing research, which focused on the energetics and mechanisms of the progression from hypertrophy to heart failure. He is using different techniques of measuring cardiac efficiency: Microcalorimetry on trabeculae and Respirometry on mitochondrial functions.
Abstract:
An increase in pulmonary arterial pressure increases the load on the right ventricle (RV). With time, progressive pulmonary arterial hypertension (PAH) results in RV hypertrophy, leading ultimately to right-heart failure. In contrast, PAH reduces the passive filling pressure in the left ventricle (LV). This reduces the LV workload, thereby resulting in LV atrophy. Does the structural deformation of the ventricles in right-heart failure affect their mechanoenergetic performance? To address this question, we used the PAH rat induced by a single injection of monocrotaline (MCT) (60 mg/kg) as our experimental model of right-heart failure. Six weeks after MCT injection, the hearts showed signs of right hypertrophy (indexed by increased free wall thickness) and left atrophy. Trabeculae tissue isolated from both ventricles of ‘Control’ and ‘PAH’ rats were mounted in our work-loop calorimeter, and subjected to stress-length work-loops over a wide range of afterloads while contracting at 5 Hz at 37 °C – a protocol designed to mimic the pressure-volume work of the heart. By simultaneously measuring heat production, mechanical efficiency was calculated as the ratio of work output to change of enthalpy (the sum of work and heat). The trabeculae were then required to undergo a preshortening protocol in which isometric force and heat output were measured as functions of muscle length. In right-heart failure secondary to pulmonary hypertension, RV trabeculae show a decrease in myocardial mechanical efficiency correlated with their lower stress-length work performance. The higher activation heat (ordinate of the heat-stress relationship) observed in RV trabeculae from the PAH group reflects an increased energy cost of Ca2+ cycling during contraction. In contrast, LV trabeculae from PAH group sustain normal energy efficiency over a wide range of afterloads.
- Workshop
Location: Amsterdam, Netherlands
Session Introduction
Louis Peeters
Utrecht University, Netherlands
Title: Pathophysiology of Hypertensive Disorders of Pregnancy (HDPs): Current insights

Biography:
Louis Peeters dedicated most of his scientific career to the study of maternal physiology in pregnancy and of the pathophysiology of hyperten- sive pregnancy disorders, both in animals and women. He started his career in 1974 with a fellowship in Fetal & Maternal Medicine at the Un. of Colorado, Denver. After his residency in Ob/Gyn. (1976-1981, Nijmegen, the Netherlands), he worked at the Dept. of Ob/Gyn., Erasmus Univ., Rotterdam and from 1987 at the Dept of Ob/Gyn, MUMC, Maastricht. In 1987 and 2001/2002, resp., he interrupted his work in the Netherlands for sabbaticals at Columbia Univ, New York City (Dept. Physiology) and UCSF, San Francisco (Dept. Ob/Gyn.). From 2011 he worked at the Dept. Ob., UMC Utrecht, to retire from clinical duties in 2013. Afterwards he continued his work in education and research. During his career he published over 150 scientific articles and over 20 book chapters.
Abstract:
Introduction: Current management of HDPs is symptomatic intended to 1) prevent deterioration of unstable cardiovascular and renal functions, and 2) minimize the infant’s risk of permanent hypoxia/prematurity- related damage. Since ≈1980 our insight in the normal and abnormal cardiovascular and volume responses to normal and HDP-pregnancies has improved markedly, offering options to develop more causal and with it, probably more effective HDP management strategies.
This lecture summarizes current insights in the mechanisms orchestrating maternal cardiovascular/volume responses to pregnancy, and with it, provides clues when and how these normal adaptations deteriorate allowing HDP to develop.
Normal cardiovascular adaptation: Within 10 days after embryo im- plantation, plasma osmolality (fig. 1) and arterial blood pressure [2] fall abruptly, probably echoing the hemodynamic effects of systemic vascular relaxation and associated fall in cardiac pre- and afterload. They trigger adaptations, which serve to secure circulatory functional integrity. Cardiac preload is restored by endocrine-induced plasma volume expansion along with the concomitant development of a more negative intrathoracic (suction) pressure. Cardiac afterload is restored by a rise in cardiac output (CO) via a baroreceptor-mediated rise in cardiovascular sympathetic tone. Preservation of the balance between cardiac pre- and afterload is pivotal for optimal cardiac function all through pregnancy (3, 4, 5).
Defective cardiovascular adaptation: Inherent to HDPs being defined by clinical signs is the heterogeneity of its preclinical pathophysiologic course. Nowadays, it is customary to differentiate between early- and late-onset HDP, primarily as they require a different clinical manage- ment. As a rule of thumb, physiologic adaptation to pregnancy deterio- rates when the balance between cardiac pre- and afterload becomes disturbed, necessitating a higher sympathetic contribution to the auto- nomic regulation of the circulatory function to preserve cardiovascular functional integrity, though, at the cost of the uteroplacental perfusion and with it, the growth of the placental functional capacity.
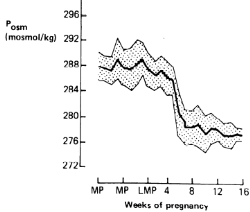
Figure 1: Weekly plasma osmolality (Posmol ± SD) before and during early pregnancy in 9 healthy pregnancies. MP and LMP indicate menstrual and last menstrual periods, respectively.
References:
- Davison JM et al, Plasma osmolality and urinary concentration and dilution during/after pregnancy. Brit J Obstet Gynaecol 1981;88:472.
- Spaanderman ME et al, The effect of pregnancy on the compliance of large arteries and veins in normal parous controls and formerly preeclamptics. Am J Obstet Gynecol 2000; 183: 1278.
- Valdes G et al. Challenges posed to the maternal circulation by preg- nancy (review). Integrated Blood Pressure Control 2011; 4: 45.
- Melchiorre K et al. Cardiac structure & function in normal pregnancy.Curr. Opin. Obstet. Gynaecol. 2012; 24: 413.
- Chung E et al. Pregnancy as a cardiac stress model. Cardiovasc. Res. 2014; 101: 561-570.
Marc Spaanderman
Maastricht University, Netherlands
Title: Risk group identification, prevention and early detection of Hypertensive Disorders of Pregnancy (HDP)

Biography:
Marc Spaanderman, MD PhD, is chair of the department of Obstetrics Maastricht University Medical Center MUMC. The past 20 years, his research group focusses on maternal health and the capacity to balance cardiovascular stress before, during and after pregnancy. As expertise center, his department structures its care around this topic in order to personalize treatment in an attempt to prevent future health problems during pregnancy and thereafter. Ways to improve patient empowerment and participation in individuals’ care are central themes in the departments’ health promoting programs. As initiator and president of the Limburg Obstetric Consortium, an obstetric-midwifery-maternity care and neonatology collaboration, he stands for structured and uniformly supplied transparent care for pregnant women and thereafter.
Abstract:
Statement of the problem: Vascular complications may arise from pre-existing cardiovascular risk factors that lower the capability to withhold the increased hemodynamic mechanical and biochemical burden of gestation or from reduced physiological adaptive capability during the first half of gestation. Although the biological diversity in jeopardizing actions of associate risk factors implies tailored preventive measures, so far, most developed preventive strategies are rather generic than specific. Systematic risk analysis of those having encountered vascular complications throughout gestation may shed light on underlying dis-orders and with it tailored preventive strategies (Fig 1). Moreover, early-pregnancy maternal adaptive responses may additionally identify those at increased risk.
Methodology and theoretical orientation: Prior to pregnancy, short sys-tematic evaluation of associated risk factors consistent with the metabolic syndrome and larger evaluation in those with prior vascular complicated pregnancy or preexisting disease associated with gestational vascular disorders may detect those at increased risk. Circulatory follow-up throughout the first half of gestation could be helpful in detecting those failing to circulatory adjust properly, increasing their risk additionally.
Findings: Generic preventive measures, such as aspirin and calcium, should be discussed in those with anticipated increased risk. Precision medication should be offered to those with serious underlying disorders as SLE and antiphospholipid syndrome, kidney disease, prior thrombotic events, chronic hypertension or cardiac failure. In order to improve maternal outcome, antihypertensive drugs should be instituted at the level of mild to moderate hypertension throughout gestation.
Conclusion and significance: Vascular complications in pregnancy may arise from preexisting cardiovascular, cardio-metabolic, hemostatic or autoimmunological risk factors. Besides generic preventive actions, precision measures can be discussed and taken depending on personal underlying disorders.
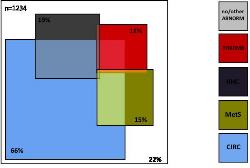
Figure 1; underlying hemodynamic, metabolic and hemostatic risk factors in 1234 non-pregnant formerly preeclampic women. (Adapted and modi-fied from reference 1)
References:
- Scholten R et al. Co-occurrence of cardiovascular and prothrombotic risk factors in women with a history of preeclampsia. Obstet Gynecol. 2013 Jan;121(1):97-105.
- Roberge S et al. The role of aspirin dose on the prevention of pre-eclampsia and fetal growth restriction: systematic review and meta-analysis. Am J Obstet Gynecol. 2016: S0002-9378(16) 30783-9.
- Hofmeyr G et al. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2014 Jun 24;(6):CD001059.
- Abalos E et al. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database Syst Rev. 2014 Feb6;(2): CD002252.
- Magee L et al. Less-tight versus tight control of hypertension in preg-nancy. N Engl J Med. 2015 Jan 29;372(5):407-17.
Johannes J. (Hans) Duvekot
Erasmus University, Netherlands
Title: Current management of Hypertensive Disorders of Pregnancy (HDPs)

Biography:
Johannes J. (Hans) Duvekot is a consultant in obstetrics and perinatology at the Erasmus MC, University Medical Center in Rotterdam, the Netherlands. In his clinical career, which started in 1984, he dedicated himself to the study of maternal hemodynamics and related disturbances like preeclampsia. During his residency at the University Hospital of Maastricht, he wrote his thesis on early changes in maternal hemodynamics and volume homeostasis. He participated in the Magpie trial that formed a milestone in prevention of eclampsia. Since 2003 he is working at the Erasmus MC in Rotterdam, where he is involved in clinical studies on preeclampsia and the long-term effects of this disease on women. He published over 150 scientific articles and over 15 book chapters.
Abstract:
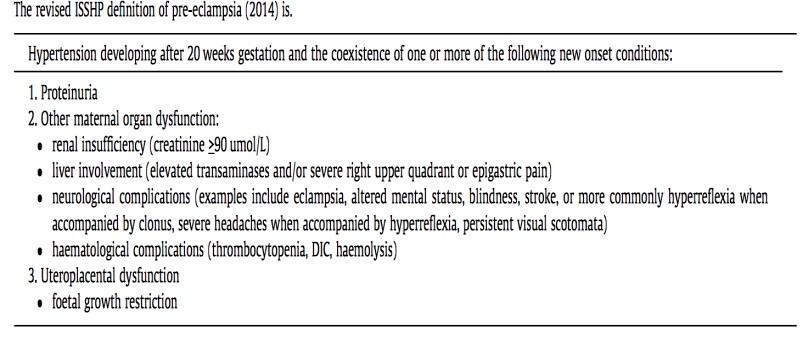
Introduction: Between 2 and 8% of pregnancies are complicated by preeclampsia (PE) defined as specified in table 1(1). At present, the only ultimate “cure” of PE and other forms of HDPs is removal of the placenta and thus, delivery. As the clinician provides “combined care” to 2 risk patients, treatment focuses on prevention of both maternal and fetal morbidity. In ≈1/3 of cases the dilemma arises that the prematurity risk outweighs maternal risks of ongoing HDP pregnancy. In ≈2/3 of cases, HDP symptoms develop >36 weeks with acceptable prematurity risks for the infant. However, at this later gestational age maternal risks are not lower! Most maternal deaths occur in the last half of pregnancy, even though the incidence of maternal death is 20-fold higher in early- onset PE. The latter is related to the much higher incidence of severe disease in early-onset PE. In developed countries PE accounts for ≈19% of maternal deaths (2).
Acute treatment: Severe HDP ought to be treated by a multidisciplinary team (obstetrician, neonatologist, and anesthesiologist). Initially, prompt stabilization by controlling blood pressure along with MgSO4 admini- stration to prevent eclampsia is of utmost importance. In most cases intra- venous administration of antihypertensives is needed. After reaching a clinically stable maternal condition, the clinician has to decide how and when to deliver the infant (2).
Temporizing management or not: In severe HDP temporizing manage- ment is only recommended after the 24th week. The best management of severe HDP between 28 and 34 weeks is still open to debate. After 34 weeks it is generally accepted to deliver women with severe HDP shortly after maternal stabilization. Between 34 and 37 weeks, temporizing management of mild HDP may be especially beneficial for the fetus (3). After 37 weeks induction of labor or elective cesarean section is strongly recommended (4). In the decision whether or not to prolong pregnancy, evaluation by a risk score may help to decide. The so-called “full-Piers” model gives some important clues for pending morbidity (5).
Table 1 (adopted from ref 1).
References:
-
Tranquilli A et al. The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. Pregnancy Hypertens 2014; 4: 97.
-
Steegers E et al. Pre-eclampsia. Lancet 2010; 376: 631.
-
Broekhuijsen K et al (HYPITAT-II study group). Immediate delivery versus expectant monitoring for hypertensive disorders of pregnancy between 34 and 37 weeks of gestation (HYPITAT-II): an open-label randomized controlled trial. Lancet 2015; 385: 2492.
-
Koopmans C et al. (HYPITAT study group). Induction of labour versus expectant monitoring for gestational hypertension or mild pre- eclampsia after 36 weeks' gestation (HYPITAT): a multicentre, open- label randomised controlled trial. Lancet 2009; 374: 979.
- von Dadelszen P et al. (PIERS Study Group.. Prediction of adverse maternal outcomes in pre-eclampsia: development and validation of the full PIERS model. Lancet 2011; 377: 219.
Johannes J. (Hans) Duvekot
Erasmus University, Netherlands
Title: Current management of Hypertensive Disorders of Pregnancy (HDPs)

Biography:
Johannes J. (Hans) Duvekot is a consultant in obstetrics and perinatology at the Erasmus MC, University Medical Center in Rotterdam, the Netherlands. In his clinical career, which started in 1984, he dedicated himself to the study of maternal hemodynamics and related disturbances like preeclampsia. During his residency at the University Hospital of Maastricht, he wrote his thesis on early changes in maternal hemodynamics and volume homeostasis. He participated in the Magpie trial that formed a milestone in prevention of eclampsia. Since 2003 he is working at the Erasmus MC in Rotterdam, where he is involved in clinical studies on preeclampsia and the long-term effects of this disease on women. He published over 150 scientific articles and over 15 book chapters.
Abstract:
Introduction: Between 2 and 8% of pregnancies are complicated by preeclampsia (PE) defined as specified in table 1(1). At present, the only ultimate “cure” of PE and other forms of HDPs is removal of the placenta and thus, delivery. As the clinician provides “combined care” to 2 risk patients, treatment focuses on prevention of both maternal and fetal morbidity. In ≈1/3 of cases the dilemma arises that the prematurity risk outweighs maternal risks of ongoing HDP pregnancy. In ≈2/3 of cases, HDP symptoms develop >36 weeks with acceptable prematurity risks for the infant. However, at this later gestational age maternal risks are not lower! Most maternal deaths occur in the last half of pregnancy, even though the incidence of maternal death is 20-fold higher in early- onset PE. The latter is related to the much higher incidence of severe disease in early-onset PE. In developed countries PE accounts for ≈19% of maternal deaths (2).
Acute treatment: Severe HDP ought to be treated by a multidisciplinary team (obstetrician, neonatologist, and anesthesiologist). Initially, prompt stabilization by controlling blood pressure along with MgSO4 admini- stration to prevent eclampsia is of utmost importance. In most cases intra- venous administration of antihypertensives is needed. After reaching a clinically stable maternal condition, the clinician has to decide how and when to deliver the infant (2).
Temporizing management or not: In severe HDP temporizing manage- ment is only recommended after the 24th week. The best management of severe HDP between 28 and 34 weeks is still open to debate. After 34 weeks it is generally accepted to deliver women with severe HDP shortly after maternal stabilization. Between 34 and 37 weeks, temporizing management of mild HDP may be especially beneficial for the fetus (3). After 37 weeks induction of labor or elective cesarean section is strongly recommended (4). In the decision whether or not to prolong pregnancy, evaluation by a risk score may help to decide. The so-called “full-Piers” model gives some important clues for pending morbidity (5)
Peter de Leeuw
Maastricht University , Netherlands
Title: Options for novel, pathophysiology-based management of Hypertensive Disorders of Pregnancy (HDPs)

Biography:
Peter de Leeuw is emeritus professor of Medicine at the Maastricht University Medical Center. His clinical and research interest goes to vascular me-dicine with particular reference to hypertension and related disorders. He has published over 700 papers on hemodynamics, neurohumoral abnor-malities and drug treatment in hypertension. Most recently, he has been involved with baroreceptor stimulation as a novel treatment of resistant hy-pertension. He has been President of the Dutch Hypertension Society and a Council Member of the International Society of Hypertension. Moreover, he has been Editor-in-Chief of three medical journals in internal medicine.
Abstract:
Introduction: From a hemodynamic point of view, hypertension may be caused by an increase in cardiac output and/or peripheral vascular resistance. In addition, volume status and the degree of vascular stiffness determine the height of blood pressure. When hypertension is found during preg-nancy (HDPs), all these pathophysiological phenomena may play a role but the pattern is far from homogeneous. First, it makes a difference whether hypertension was pre-existent or induced by the pregnancy. Secondly, it is important to consider that HDP may involve as a spon-taneous disorder in an otherwise healthy woman or be superimposed upon another ‘silent’ underlying abnormality.
Pathophysiological considerations: In pregnancy-related hypertension we usually find a lower cardiac output, increased vascular resistance, increased arterial stiffness and a reduced plasma volume. The activity of the renin-angiotensin system is suppressed as well. This suggests that there is a hypertensive stimulus which leads to a compensatory reduction in pressor systems. The fact that sympathetic activity is activated rather than suppressed can be seen as an attempt to ‘keep the circulation going’.
Pathophysiology-based management: The most appropriate approach to the patient with a HDP is to direct treatment to those factors that could initiate or exacerbate a rise in pressure. Recent evidence suggests that a substantial proportion of women with preeclampsia - a common form of HDP - have renal vascular abnormalities, either as a pattern of intrarenal nephrosclerosis or, and perhaps more often, as macrovascular disease, notably fibromus-cular dysplasia.
References:
- Vance CJ et al. Increased prevalence of preeclampsia among wo-men undergoing procedural intervention for renal artery fibro-muscular dysplasia. Ann Vasc Surg 2015; 29: 1105.
- Spaanderman ME et al, The effect of pregnancy on the compliance of large arteries and veins in normal parous controls and formerly preeclamptics. Am J Obstet Gynecol 2000; 183: 1278.
- Abalos E et al. Antihypertensive drug therapy for mild to mode-rate hypertension during pregnancy. Cochrane Database Syst Rev. 2014 Feb6;(2): CD002252.
- Van Twist DJ et al. Renal hemodynamics and renin-angiotensin sys-tem activity in humans with multifocal renal artery fibromuscular dysplasia. J Hypertens 2016; 34: 1160.
- De Leeuw PW et al. Bilateral or unilateral stimulation for baroreflex activation therapy. Hypertension 2015; 65: 187.
- Workshop
Location: Amsterdam, Netherlands
Session Introduction
Hossein Tabriziani
Loma linda University, USA
Title: Hypertension & cardiovascular disease after kidney transplantation
Time : 12:10-13:10

Biography:
Dr. Tabriziani has earned his MD with honors from Iran University of Medical Sciences (IUMS). He finished his Internal Medicine residency at St. Barnabas Hospital, Weill Cornell Medical College in New York. With passion for education and Transplantation, he accepted the fellowship in Nehrology and Hypertension at Georgetown University in Washington, DC and continued his education at University of California San Francisco (UCSF) with a Transplant Nephrology fellowship. He was appointed at the Medical director of Pancreas Transplantation at Westchester Medical Center, New York Medical college before moving to Loma Linda University in California to serve as an Assistant Professor of Medicine in Nephrology / Transplant division. He is an active member of American Society of Nephrology and American society of Transplantation. His interests are in Hypertension and Oxidative Stress in patients with chronic kidney disease and transplantation.
Abstract:
The incidence of End Stage Renal Disease (ESRD) continues to rise in the United States. By the year 2030, the number of patients with ESRD is projected to exceed 2.2 million. This is more than five times the current prevalence.
During the past decade, kidney transplantation has increasingly been recognized as the treatment of choice for medically suitable patients with ESRD. As well as improving quality of life, successful transplantation confers major benefits by improving morbidity and mortality of ESRD patients who receive kidney transplant over those who undergo Renal Replacement Therapy (RRT). Cardiovascular (CV) risk reduction remains the leading cause of this improvement, although both modalities provide compatible fluid balance and glomerular filtration.
As the United States Renal Data System (USRDS) shows, mortality is improved significantly for ESRD patients who received renal transplantation as compared to those with RRT.
Oxidative stress plays a key role in the pathophysiological process of uremia and its complications, particularly in cardiovascular disease. The level of oxidative stress markers is known to increase as Chronic Kidney Disease (CKD) progresses and correlates significantly with level of renal function.
Successful kidney transplantation, results in near normalization of the antioxidant status and lipid metabolism by eliminating free radicals despite the surge of oxidative stress caused by the surgical procedure and ischemic injury to the organ during the operation. This success is associated with both improved renal function, reduced cardiovascular complications, and overall improved morbidity and mortality.
Fabiola B Sozzi
University of Milan, Italy
Title: Unexplained dyspnea and diastolic function
Time : 15:10-16:00

Biography:
Fabiola Sozzi works as a staff cardiologist at the University Hospital Policlinico of Milan, Italy, with high-specialization nomination. She has high skills in multimodality imaging of heart disease using echocardiography integrated with cardiac magnetic resonance imaging, cardiac computed tomography and nuclear. She also works in the acute clinical setting treating acute cardiac syndromes. She gained a high expertise in echocardiography at the Thoraxcentre of Rotterdam (NL), where she defended the PhD thesis on stress cardiac imaging under the supervision of Professor J. Roelandt. She is Visiting Professor at the University of Milan where she leads several research projects and teaches at the Faculty of Medicine and School of Specialization of Cardiology. She is author of 70 papers published in indexed peer-reviewed international journals and reviewer of several medical international journals.
Abstract:
Chronic dyspnea is associated with a variety of diseases and is also a major symptom of heart failure (HF). The differential diagnosis of dyspnea is a daily routine in every cardiology practice. Approximately one-half of patients with HF have a preserved ejection fraction (HFpEF). Diagnosis of HFpEF is challenging and relies largely on demonstration of elevated cardiac filling pressures represented by the pulmonary capillary wedge pressure (1). The American College of Cardiology Foundation/American Heart Association guidelines define HFpEF as clinical signs and symptoms of HF, preserved ejection fraction, and no other obvious explanation for symptoms. This scheme works well for patients with a high likelihood of disease on the basis of clinical indicators of congestion. To address the patients without overt congestion, more recent guideline statements from the European Society of Cardiology (ESC) and American Society of Echocardiography/European Association of Cardiovascular Imaging (ASE/EACVI) [2] require objective evidence of high left ventricular filling pressures. Elevated left ventricular filling pressure is a cardinal feature of HfpEF and can be clinically demonstrated by elevations in plasma natriuretic peptide levels. The ratio of transmitral E to mitral annular e′ velocities (E/e′) at doppler echocardiography has been proposed as a non-invasive measure of left ventricular filling pressure and endorsed by professional guidelines as a surrogate parameter of invasive left ventricular filling pressure in the diagnostic work-up of HFpEF.
The diagnosis of HFpEF is straightforward when patients are acutely decompensated. To make matters more complex, many patients with HFpEF display normal left ventricular filling pressures at rest, with abnormalities that develop during stresses like exercise (3). Invasive hemodynamic exercise testing has emerged as the gold standard to diagnose or exclude HFpEF in patients with exertional dyspnea of unclear etiology, but cost, risk, and the requirement for specialized training and equipment may limit its broad application in practice and in clinical trials. Therefore, doppler echocardiography plays a central role in the non-invasive evaluation and grading of diastolic dysfunction.
References:
- Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelisa A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009; 10:165-193.
- Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur Heart J. 2011;32:670-679.
- Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200.
- Posters
Location: Amsterdam, Netherlands
Session Introduction
Hsuan Lo
Tzu University, Taiwan
Title: Altered NMDA receptor-nitric oxide (NO) signaling in the rostral ventrolateral medulla contribute to cardiovascular response of acute ethanol-exposure

Biography:
Hsuan Lo is a PhD scholar, studied in the Department of Pharmacology and Toxicology at Tzu Chi University. His lab is interested in neuropharmacology particularly in alcohol effects on the central nervous system and cardiovascular function. His studies focus on the mechanism of acute ethanol intake action on the glutamate signaling within the rostral ventral lateral medulla (RVLM). He has performed the whole animal model with practiced skill in RVLM, microinjection of drug and femoral artery surgery for measuring blood pressure, and also have set up the HPLC system to detect the neurotransmitter content. On the other hand, his master's thesis was of Amyloid-beta peptides on NMDA receptor activation in rat sympathetic preganglionic neurons using whole cell, patch clamp technique. All his training has led him to know more about, how the CNS works to control cardiovascular function.
Abstract:
Consumption of ethanol (EtOH) has many effects on physiological functions particular in the central nerve system and cardiovascular system. Hypotension is one of the main features of acute excessive intake of ethanol (alcohol intoxication). In addition, chronic ethanol consumption has been associated with cardiovascular diseases, including hypertension and stroke. The precise mechanisms underlying ethanol regulation of cardiovascular function remains unclear. It is well known that central N-Methyl-D-Aspartate (NMDA) receptors are implicated in the modulation of glutamatergic transmission and
important in regulating neuronal activity. Recent evidence also suggests that nitric oxide is a key neuromodulator within the central nervous system and its production is associated with NMDA receptor activation. The rostral ventrolateral medulla (RVLM) is known as a vasomotor center, which provides the basal sympathetic outflow and maintains blood pressure (BP). This study was carried out to test the hypothesis that NMDA and NO signaling in the RVLM are involved in the regulation of ethanol-induced changes in BP. The BP response was measured in urethane anesthetized SD rats weighing 280-350 g. EtOH (3.2 g/kg) was applied by intraperitoneal injection (IP). The samples of glutamate and NO were collected by micro dialysis every 15 minutes in the RVLM and then analyzed with HPLC-ECD and NOx analyzer, respectively. The results showed that IP ethanol elicited a significant increase in the level of glutamate and NO in RVLM and a reduction in BP. Microinjection of ketamine (an NMDA receptor antagonist) or L-NNA (an NOS inhibitor) into the RVLM, which was applied 5 min after administration of EtOH, attenuated EtOH-induced depressor effects. In addition, microinjection of ketamine suppressed the level of NO production. The results suggest that increases in NMDA receptors activation and enhancement of NO synthase activity in the RVLM may play a major role in ethanol-evoked hypotension.
